NRH News
Antibiotic Awareness

- Antibiotics can save lives. When a patient needs antibiotics, the benefits outweigh the risks of side effects and antimicrobial resistance.
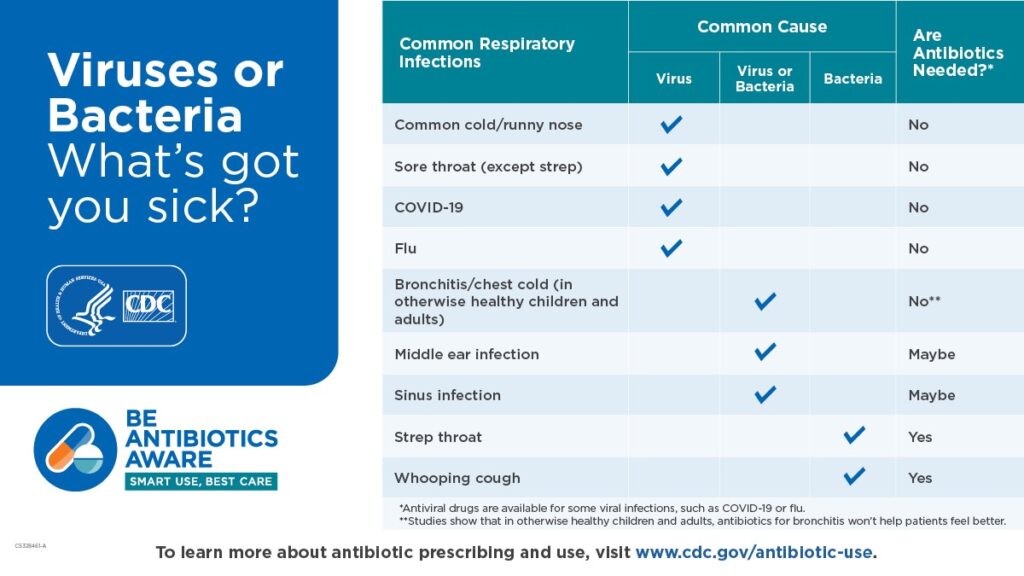
- Antibiotics do NOT treat viruses, like those that cause colds, flu, respiratory syncytial virus (RSV), or COVID-19. Other medications, like antivirals, can treat viruses.
- Antibiotics are only needed for treating certain infections caused by bacteria, but even some bacterial infections get better without antibiotics. Antibiotics are not needed for treating many sinus infections and some ear infections, which can be caused by either bacteria or viruses.
- An antibiotic will not make you feel better if you have a virus. Respiratory viruses usually go away in a week or two without treatment. Ask your healthcare professional about the best way to feel better while your body fights off the virus.
- When antibiotics aren’t needed, they won’t help you, and the side effects could still cause harm. Side effects range from minor to very severe health problems. When you need antibiotics for a bacterial infection, the benefits usually outweigh the risk of side effects.
- Taking antibiotics can contribute to the development of antimicrobial resistance. Antimicrobial resistance occurs when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. If antibiotics and antifungals lose their effectiveness, then we lose the ability to treat infections, like those that can lead to sepsis.
- If you need antibiotics, take them exactly as prescribed. Talk with your healthcare professional if you have any questions about your antibiotics.
- Talk with your healthcare professional if you develop any side effects, especially severe diarrhea, which could be Clostridioides difficile (or C. diff ) infection, a condition that requires immediate treatment.
- Do your best to stay healthy and keep others healthy. This helps reduce antibiotic use and fights antimicrobial resistance:
- Clean your hands by washing with soap and water for at least 20 seconds or using a hand sanitizer that contains at least 60% alcohol.
- Cover your coughs and sneezes with a tissue.
- Stay at home when sick.
- Avoid touching your face.
- Avoid close contact with people who are sick.
- Get recommended vaccines, such as the flu and COVID-19 vaccines.
- If you need antibiotics, take them exactly as prescribed.
- Antibiotics aren’t always the answer. Everyone can help improve antibiotic use. Improving the way we take antibiotics helps keep us healthy now, helps fight antimicrobial resistance, and ensures that these life-saving antibiotics will be available for future generations.
Messages about Antimicrobial Resistance
- Antibiotics can save lives, but any time antibiotics are used, they can cause side effects and contribute to the development of antimicrobial resistance.
- Antimicrobial resistance happens when germs, like bacteria and fungi, develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow.
- Antimicrobial resistance is an urgent global public health threat, killing at least 1.27 million people worldwide and associated with nearly 5 million deaths in 2019.
- In the U.S., more than 2.8 million antimicrobial-resistant infections occur each year, and more than 35,000 people die as a result. (See CDC’s antimicrobial resistance website).
- In addition, 202,600 hospitalized cases of Clostridioides difficile (or C. diff ) occurred in 2019 and at least 11,500 people died. C. diff is rarely resistant to antibiotics; however, it usually occurs in people who have taken antibiotics.
- Antimicrobial resistance does not mean the body is resistant to antibiotics or antifungals; it means bacteria and fungi that live in and on our bodies develop the ability to defeat the drugs designed to kill them.
- When bacteria become resistant, antibiotics cannot fight them, and the bacteria multiply.
- Antimicrobial-resistant infections can be difficult, and sometimes impossible, to treat.
- Antimicrobial-resistant germs can quickly spread across settings, including communities, the food supply, healthcare facilities, the environment (e.g., soil, water), and around the world. Antimicrobial resistance is a One Health problem—the health of people is connected to the health of animals and the environment (soil, water).
Additional CDC Resources
Antibiotics Quiz
- Be an antibiotics whiz. Test your knowledge about antibiotics.
Stewardship Report
- Current Report: Antibiotic Use in the United States: Progress and Opportunities
- Past Antibiotic Prescribing and Use Reports
Spanish Resources
Information for patients on antibiotic use and resistance in Spanish (Recursos educativos para pacientes y profesionales de atención médica.)
Related Articles
Newman Regional Health Enhances Patient Portal with New Features for Easier Access to Health Records
Newman Regional Health is excited to announce significant updates to their patient portal, MHealth, powered by MEDITECH Expanse. These enhancements make it even easier…
Newman Regional Health Earns Reaccreditation from the American College of Cardiology
Newman Regional Health is proud to announce its reaccreditation for Percutaneous Coronary Intervention (PCI) from the American College of Cardiology…
Summer Nurse Externship Program
Our Nurse Externship program provides a summer learning experience tor college students who have completed their junior year of nursing…

